The Shoulder Center
Expertise in SHOULDER Conditions & Procedures
SHOULDER PAIN
The shoulder is an extraordinary joint, allowing up to 180-degrees of motion in 3 different planes. But, the more that it can do, the more that can go wrong! Boston Orthopaedic & Spine physicians have the expertise and experience to provide comprehensive care of the shoulder including nonsurgical treatments, arthroscopic, and open surgeries.
COMMON SHOULDER CONDITIONS
Since your shoulder is such a complex joint, there are many conditions that can cause pain and limit function. Some of the most common conditions include:
- Rotator cuff tear
- Frozen shoulder
- Instability
- Bursitis
- Arthritis
- Dislocation
- Labral tear
- SLAP tear
- Fractures
Whether you have had pain for years, or the symptoms recently started to affect your life, we are here to help.
TREATMENTS
Most patients do not need surgery to manage their shoulder pain. At Boston Orthopaedic & Spine, we find that most shoulder pain is successfully managed with conservative measures such as rest, anti-inflammatory medications, ice/heat, stretching, injections, and physical therapy.
When nonsurgical options fail to relieve pain and restore function, our board-certified, fellowship-trained orthopedic surgeons are highly skilled with arthroscopic and open procedures.
- Shoulder arthroscopy – During arthroscopy, the surgeon with use small portals to insert a camera and instruments into your shoulder. This minimally invasive approach allows for faster healing and a more rapid recovery.
- Shoulder arthroplasty – Arthroplasty, or replacement, is reserved for advanced arthritis of the shoulder after failing conservative treatment. Our team of experts has performed hundreds of total and reverse total shoulder replacements to restore patients to activity.
Common Shoulder Conditions
The shoulder is a very complex part of the body, and when one component is not working properly, the result is pain and dysfunction. At Boston Orthopaedic & Spine, our team of board-certified, fellowship-trained experts understands this complex joint, and they have the training and expertise to return you to your active life.
SHOULDER ANATOMY
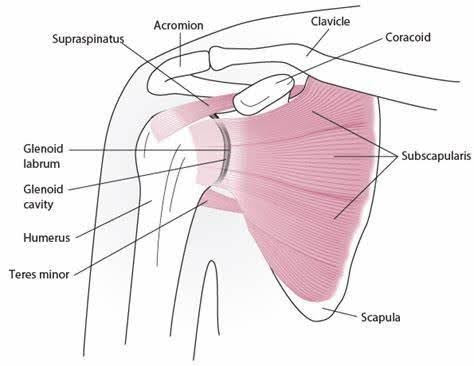
The shoulder is made up of three bones: the scapula (shoulder blade), the humerus (upper arm bone) and the clavicle (collarbone). Connecting these are ligaments and tendons.
- The part of the scapula that makes up the roof of the shoulder is called the acromion.
- The joint where the acromion and the clavicle join together is known as the acromioclavicular (AC) joint.
- The true shoulder joint is called the glenohumeral joint and consists humeral head and the glenoid. It is a ball and socket joint.
- The rotator cuff muscles and their tendons play an important role in the correct functioning of this joint. They are responsible for the motion, stability, and power of the humerus. 4 tendons join to make up the rotator cuff.
- The labrum surrounds the glenoid and deepens the socket. It aids in stability.
COMMON CAUSES OF SHOULDER PAIN AND INJURY TREATED AT BOSTON ORTHOPAEDIC & SPINE
Arthritis
Arthritis, or osteoarthritis, is loss of cartilage within a joint. While there are many other types of arthritis, including rheumatoid, psoriatic, septic, post-traumatic, and lupus, wear and tear osteoarthritis remains by far the most common. Arthritis symptoms can include swelling, tenderness, sharp pain, stiffness, and sometimes fever and chills.
Bursitis
Bursitis is painful inflammation of the bursae, the fluid-filled sacs that reduce friction between bones, tendons, and muscles. Bursitis in the shoulder is commonly caused by an injury, infection or other condition. Pain may be accompanied by swelling, tenderness or loss of movement. Treatment is rest, ice, activity modifications, injections, and in some cases, surgery.
Dislocated shoulder
A dislocated shoulder occurs when the upper arm bone (humerus) is forced out of its natural position inside the shoulder socket. Symptoms include severe pain, swelling, bruising, and a visible deformity of the shoulder.
A dislocation is a serious injury that requires medical attention. A physician will put the arm bone back into the socket either manually or surgically. The joint will be immobilized in a sling, and medication may be prescribed to help manage the pain. In the early stages after a dislocation, physical therapy is helpful to restore the shoulder stability. If instability persists, surgery is often indicated.
Rotator Cuff Tear
A rotator cuff tear is an injury to any of the four rotator cuff tendons in the shoulder. Tears are caused by repetitive motion or sudden injury.
Symptoms include pain, weakness in the shoulder, and difficulty raising the arm overhead. Treatment for a rotator cuff tear depends on the severity of the damage, and may include rest, ice, over-the-counter pain medication, physical therapy or surgery.
Fractures
A fracture is a break in a bone. Broken bone symptoms include pain (intensified when the area is moved or pressure is applied), swelling, bruising, and loss of function. Fractures may also cause the area around the bone to appear distorted or deformed, especially in open fractures where the bone protrudes from the skin.
Frozen shoulder
Frozen shoulder, also known as adhesive capsulitis, is a condition in which the capsule of tissue surrounding the shoulder joint becomes thicker or tighter, restricting movement. Symptoms typically develop in several stages, and resolve within one or two years.
Common symptoms include pain, stiffness, and restricted range of motion. Treatment options include over-the-counter pain medication, physical therapy, or injections. Most cases of frozen shoulder go away within 18 months, but for some patients, surgery may be necessary.
Shoulder Impingement
Impingement is caused by irritation of the tendons and bursa on the bones of the shoulder. It is often caused by repetitive overhead activities or throwing sports.
Symptoms include generalized aching of the shoulder and pain when raising the arm out from the side or in front of the body. Impingement may also cause a sharp pain when trying to reach into your back pocket, or difficulty sleeping due to pain. Treatment for shoulder impingement includes rest, ice, and physical therapy. In some cases, surgery may be necessary to restore functionality.
Shoulder separation
A shoulder separation is an injury to the ligament that connects the shoulder blade (scapula) and the collarbone (clavicle). This injury can vary in severity from a strain to a complete dislocation of the acromioclavicular (AC) joint. We often see athletes in sports like football, hockey, and skiing who may experience an AC joint injury as a result of falling or being hit on the shoulder.
Symptoms include pain, tenderness, swelling, and bruising. Signs of a severe separation are a popping sensation when the loose joint shifts, and a noticeable bump on the shoulder where the collarbone has moved out of place. Treatment for shoulder separation depends on the severity of the injury, but includes anti-inflammatory medications and immobilization of the shoulder with a sling. For more severe separations, surgery may be recommended.
SLAP tear
A SLAP tear is an injury to the ring of cartilage that surrounds the shoulder socket, called the labrum. The acronym SLAP stands for superior labrum, anterior to posterior, and means that the top of the labrum is torn from back to front.
This injury is common among athletes, and often occurs when falling on the outstretched arm or the shoulder. SLAP tears can also happen as a result of repeated overhead motions or sudden heavy lifting. Symptoms include aching pain, weakness, and popping or clicking in the shoulder. Treatment for SLAP tears includes over-the-counter anti-inflammatory medicine, physical therapy, and in some cases, surgery.
Tendonitis
Tendonitis is inflammation of the tendons, the tissue that connects muscle to bone. Tendonitis is caused by overuse (repetitive motion) or sudden injury. Tendonitis symptoms include pain in the tendon area, swelling, and loss of motion.
Biceps tendonitis is inflammation of the tendons that connect the biceps muscle to the top of the shoulder. It may be caused by overuse, wear and tear from aging, or injuries to the shoulder. Sports activities like golf, tennis, and swimming can cause biceps tendonitis, as well as work activities that require frequent overhead motions.
Symptoms of bicep tendonitis include aching pain that increases with use of the arm and shoulder It may also cause weakness when bending at the elbow or twisting the arm. Treatment includes rest, over-the-counter anti-inflammatory medicine, and physical therapy. In some cases, surgery may be necessary for patients who are not improving with non-surgical treatments.
Wear and Tear
A common cause of shoulder pain is arthritis. The most common type of arthritis is osteoarthritis (OA) — sometimes called degenerative arthritis because it is a “wearing out” condition involving the breakdown of cartilage in the joints. When cartilage wears away, the bones rub against each other, causing pain and stiffness. OA usually occurs in people aged 50 years and older, and frequently in individuals with a family history of osteoarthritis.
The most common cause of shoulder replacement, OA can occur without a shoulder injury. However, this seldom happens since the shoulder is not a weight-bearing joint like the knee or hip. Instead, shoulder OA commonly occurs many years following a shoulder injury, such as a dislocation, that has led to joint instability and repeated shoulder dislocations — damaging the shoulder joint so that OA develops.
Your Treatment Options for Shoulder Pain
Following an orthopaedic evaluation of your shoulder, your doctor will review and discuss the results with you. Based on his or her diagnosis, your treatment options may include:
- Medication
- Physical therapy
- Shoulder joint fluid supplements (injections that provide temporary pain relief)
- Total shoulder joint replacement
When joint pain and stiffness become severe enough to affect your daily life and comfort, and when that pain is not relieved by other treatment options, shoulder replacement may be recommended.
Severe arthritis may lead to Shoulder Replacement Surgery.
Rotator Cuff Tear
Rotator cuff tears are common in the adult population of people over 40. The rotator cuff is made up of four muscles and their tendons, which act to hold the upper arm (humerus) to the socket of the shoulder (glenoid fossa). The rotator cuff also provides mobility and strength to the shoulder joint. Two sac-like structures, called bursae, allow smooth gliding between the bone, muscle, and tendon. They also cushion and protect the rotator-cuff structures from the upper part of the scapula (the acromion).
SYMPTOMS
Pain occurring in the front of the shoulder that radiates down the side of your arm.
GRADUAL PAIN
Gradual onset of pain is most common in the adult population. It is often caused by repetitive overhead activity or by wear and degeneration of the tendon. Activities involving reaching or lifting may bring about an onset of pain. At first the pain may be mild and relieved by over-the-counter medication such as aspirin or ibuprofen.
Over time the pain may become noticeable at rest or with no activity at all and be accompanied by stiffness and loss of motion. Simple tasks such as combing your hair or placing your arm behind your back may prove difficult and/or painful.
ACUTE PAIN
Trauma such as a lifting injury or fall can cause a tear in the rotator cuff that results in acute pain. When the tear occurs with an injury, there may be sudden acute pain, a snapping sensation and an immediate weakness of the arm.
Broken/Fractured Arm
Most people know right away if they broke their arm due to a snap or loud cracking sound, extreme pain at the site of the injury, pain increased by any movement, and / or loss of normal use of the arm. Arms often break due to a fall on an outstretched arm or major accident such as a car crash. Common fracture points include the wrist, radius (forearm), elbow, and humerous.
Trying to break a fall by putting your hand out in front of you seems almost instinctive, but the force of the fall could travel up your lower forearm bones and dislocate your elbow. It also could break the smaller bone (radius) in the forearm. The breaks can occur at the wrist (Colles fracture), or near the elbow at the radial “head.” Children are more likely to break the bones in their lower arm, which are called the radius and ulna. A direct blow to the elbow or fall on a bent elbow can cause it to break. About one in every 20 fractures involves the upper arm bone which is called the humerus.
If you have any of these signs or symptoms after a fall, see your doctor:
- Pain or swelling at the site of the injury (outside of the elbow, wrist, etc)
- Pain increased by any movement of the injured area
- Loss of normal use of the arm.
- Difficulty in bending or straightening the elbow accompanied by pain
- Inability or difficulty in turning the forearm (palm up to palm down or vice versa)
- Numbness in one or more fingers.
FIRST AID
Because breaks often occur as a result of an accident first aid is usually required.
- Make sure the injured person is out of the way of further harm.
- Check to see if they are breathing normally.
- Check their pulse.
- Call 911 if their breathing and/or pulse are irregular, if there is serious bleeding, or if there is reason to suspect multiple broken bones or other injuries.
- Elevate the injured arm above the person’s heart. This slows bleeding and reduces swelling.
- If the bone is sticking out from the skin do not try to push it back in. Instead, cover it with a clean, dry cloth or bandage.
- Do not use the broken arm. Moving the arm could cause further injury. To immobilize a broken arm:
- Make a temporary splint. Find something long and stiff to attach to the site of the injury. Wood or rolled up magazines or newspapers attached to the arm with cloth, belts or tape can be used to immobilize the joint. Make sure both ends of the splint extend far above and below the injury. Tie the splint tight enough to hold it in place, but not so tight as to reduce blood flow.
- Make a sling. Place the injured arm across the chest with the hand resting near the shoulder. Use a loop of cloth supported from the neck and around the arm to stabilize the injury and support the splint.
Take the injured person to a doctor immediately.
Recovering From a Broken Arm
The Doctor’s Visit
Tell the doctor exactly what happened. He or she will physically examine the broken arm and check for other injuries, such as nerve damage. The doctor may want to see if the patient can flex and extend the wrist and fingers. Sometimes the doctor may use X-rays or other diagnostic imaging tools to see the bones of both the injured and uninjured arms.
What to Expect
The doctor may need to move pieces of bone back into their correct positions (a process called reduction). Depending upon the severity of injury, the patient may or may not need anesthesia. Those with more serious fractures may require surgery.
Once the broken bone is back in place the arm is immobilized by placing it in a cast or splint. You will be advised how long to wear the cast or splint, and given a follow-up appointment to check on the bone healing and cast removal.
Fracture Types and Treatments
Radial head fractures are classified according to the degree of displacement (movement from the normal position).
Type I fractures are generally small, like cracks, and the bone pieces remain fitted together.
The fracture may not be visible on initial X-rays, but can usually be seen if the X-ray is taken three weeks after the injury.
Nonsurgical treatment involves using a splint or sling for a few days, followed by early motion.
If too much motion is attempted too quickly, the bones may shift and become displaced.
Type II fractures are slightly displaced and involve a larger piece of bone.
If displacement is minimal, splinting for one to two weeks, followed by range of motion exercises, is usually successful.
Small fragments may be surgically removed.
If the fragment is large and can be fitted back to the bone, the orthopaedic surgeon will first attempt to fix it with pins or screws. If this is not possible, however, the surgeon will remove the broken pieces or the radial head.
The surgeon will also correct any other soft-tissue injury, such as a torn ligament.
Type III fractures have more than three broken pieces of bone, which cannot be fitted back together for healing.
Usually, there is also significant damage to the joint and ligaments.
Surgery is always required to remove the broken bits of bone and repair the soft-tissue damage.
Early movement is necessary to avoid stiffness.
Regardless of the type of fracture or the treatment used, physical therapy will be needed before resuming full activities.
Cast Care
It’s important that you take good care of your cast during your recovery period. View more information regarding the care of your cast.
For more information see the AAOS: Elbow Fractures, Radial Head Fractures, Broken Arm
RECOVERING FROM A BROKEN ARM
Rehabilitation
It may take from several weeks to several months for the broken arm to heal completely. Rehabilitation involves gradually increasing activities to restore muscle strength, joint motion and flexibility. The patient’s cooperation is essential to the rehabilitation process by completing range of motion, strengthening and other exercises prescribed by the doctor. Rehabilitation lasts until tissues perform their functions normally. After rehabilitation, the doctor may want to see the arm again to make sure healing is complete.
Cast Care
It’s important that you take good care of your cast during your recovery period. View more information regarding the care of your cast.
Shoulder Replacement Surgery
About the Shoulder
The normal shoulder is very complex and involves three bones and more than one joint. These bones are the clavicle (collar bone), the scapula (shoulder blade), and the humerus (upper arm bone). The upper end of the arm bone (humerus) and the outside edge of the scapula bone (glenoid) form a “ball-and-socket joint.” There are numerous muscles, ligaments and tendons which help to provide stability and movement. This joint is remarkable because it typically allows for greater range of motion than any other joint in your body.
Types of Shoulder Replacements
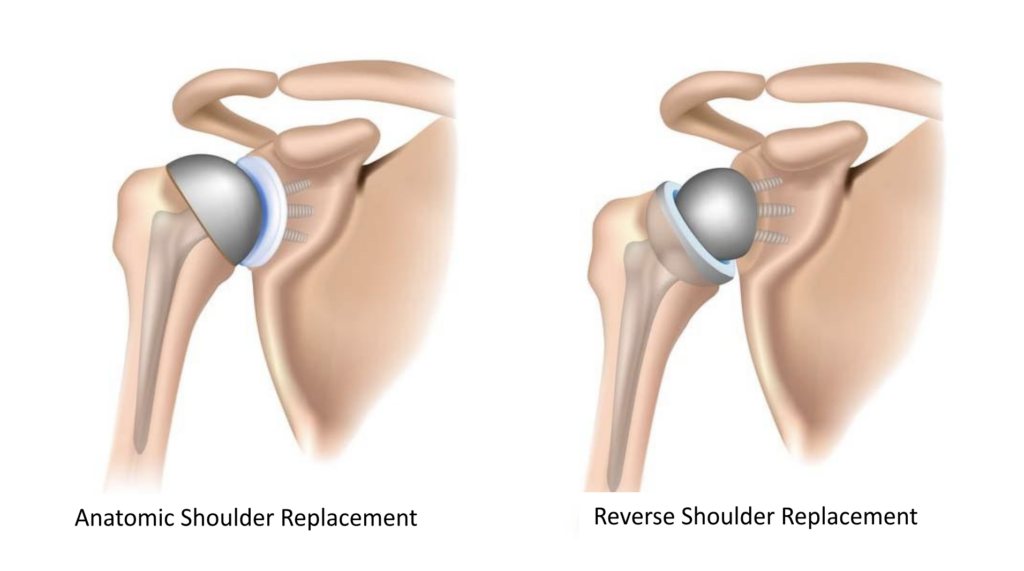
There are two types of replacements:
An “anatomic” total shoulder mimics the original anatomy of your shoulder. A metal ball replaces the end of the upper arm bone (humerus) and a plastic socket is cemented into the glenoid (part of the scapula, or shoulder blade). The rotator cuff is left intact. This type of shoulder replacement offers pain relief and improved function. Because it resembles your original anatomy and the rotator cuff is left intact, an anatomic replacement may lead to better total mobility and function than a reverse total shoulder, especially when reaching behind your back.
A “reverse” shoulder replacement reverses the alignment of implants. A metal ball replaces the glenoid and a plastic cup replaces the end of the humerus. It does not rely on an intact rotator cuff and can be used in the setting of a rotator cuff tear or even when the shoulder has been so severely fractured that the pieces cannot be put back together. Like the anatomic shoulder replacement, a reverse total should offer pain relief and significant improvement in function.
There are multiple factors that determine which implant is best suited for you.
Who Needs Total Shoulder Replacement Surgery?
Total shoulder replacement surgery can be discussed with your doctor when other nonoperative treatments have not worked or if there are no other reasonable options. Arthritis is a common cause of shoulder pain as we get older. The normal, smooth cartilage within our joints can wear away with time or after earlier trauma. As the cushion (cartilage) wears away, the force through the joint is transmitted to the bone causing pain, stiffness and swelling. Most patients who decide to have schoulder replacement surgery have experienced shoulder pain for a long time. Arthritis also causes loss of motion and function. Many patients have developed pain that limits their daily activities and may interfere with their ability to sleep. Shoulder replacement surgery can alleviate shoulder pain and improve range of motion of your shoulder joint.
What are the most common reasons for a total shoulder replacement:
Anatomic Shoulder Replacement:
- Osteoarthritis – The cartilage has worn away resulting in bone-on-bone contact.
- Avascular necrosis – in some cases, the blood supply to the proximal humers (ball) can be disrupted leading to bony cell necrosis (or cell death) and collapse of the bone underlying the cartilage cushion.
Reverse Shoulder Replacement:
Because a reverse total shoulder does not rely on an intact rotator cuff it can be used for more conditions:
- Rotator cuff tear arthropathy – when a rotator cuff tears it can become larger over time. The tear can eventually become unrepairable. Because the rotator cuff helps center the ball in the socket, when a tear is large enough the ball does not sit normally in the socket and it leads to arthritis. So this condition is both a rotator cuff tear and arthritis.
- Chronic rotator cuff tears that cannot be surgically repaired
- Severe osteoarthritis
- Rheumatoid arthritis
- Fractures of the proximal humerus or ball that are too severe for repair or reconstruction
- Revisions of failed anatomic shoulder replacements
Our Team
Thomas F. Burke, MD
Learn More
About Dr. Burke
Orthopedics Surgeon
Specializing in: Sports Medicine, Arthroscopy,
Trauma & Fracture Care, Shoulder Reconstruction
James A. Karlson, MD
Learn More
About Dr. Karlson
Orthopedic Surgeon
Specializing in Sports Medicine Including:
Knee, Hip, Ankle, and Shoulder injuries
Glen Ross, MD
Learn More
Anthony J. Schena, MD
Learn More
About Dr. Schena
Orthopedic Surgeon
Specializing in Sports Medicine, General Orthopedics (Knee, Shoulder, and Joint Reconstruction)
Take the First Step
Get an accurate diagnosis and treatment plan from our expert physician team.





